Across the United States, geography quietly shapes who survives serious injury. In mountains, deserts, wilderness corridors, and disaster-prone regions, patients with severe trauma face a simple disadvantage. Mortality in rural and frontier areas is twice that in urban areas. Blood is often not available when it is needed most.
Medical science has long shown that uncontrolled bleeding is the leading preventable cause of death after injury. What is less widely understood is how often modern trauma care fails not because of knowledge or skill, but because of distance. Blood products require refrigeration, careful handling, and time. Outside major hospitals, those requirements can become barriers that cost lives.
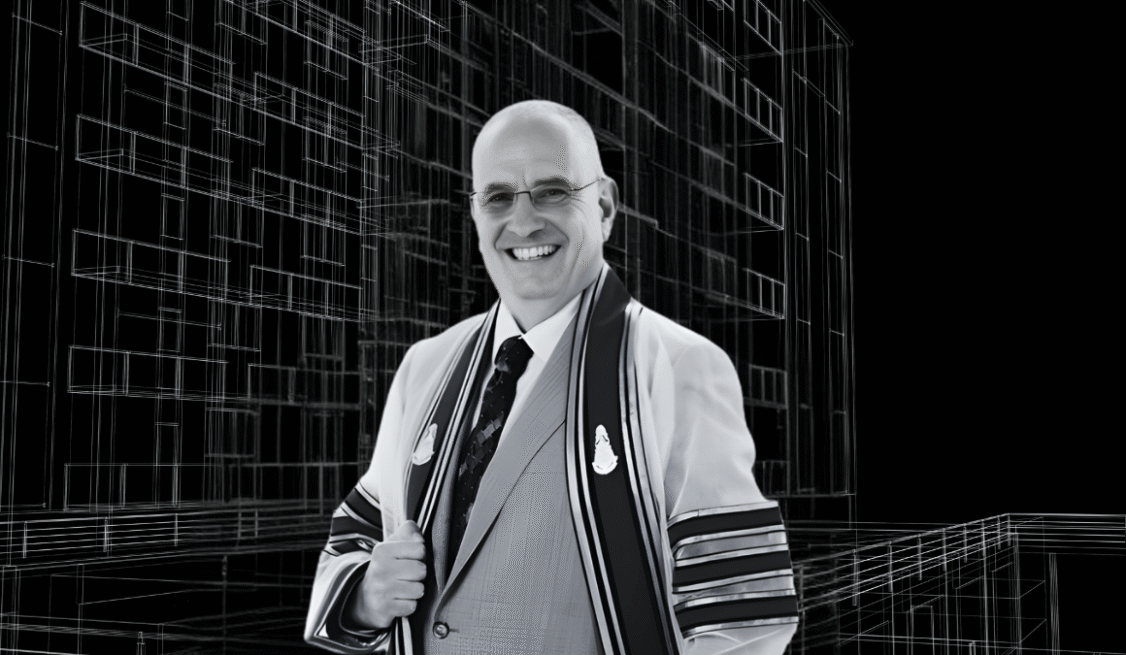
For Dr. Martin A. Schreiber, this problem has been central to decades of work in trauma medicine.
Dr. Martin Schreiber, a trauma surgeon, researcher, and U.S. Army Reserve colonel, has spent his career confronting the limits of emergency care in environments where hospitals are hours away. Martin Schreiber, MD, known nationally for his leadership in trauma resuscitation science, has shaped how blood products are used in both civilian and military medicine.
Currently, he is part of the team of researchers investigating the potential impact of dried blood products.
In a 2025 review published in the journal Transfusion, Dr. Martin A. Schreiber and co-author Alexandra M.P. Brito outline the growing evidence behind freeze-dried and spray-dried plasma. These products can be stored at room temperature, carried easily, and reconstituted with sterile water in minutes. For patients bleeding far from definitive care, that difference could be decisive.
The logic is straightforward. Plasma contains clotting factors that help stop hemorrhage and stabilize circulation. In hospitals, plasma is frozen, thawed, and transfused under controlled conditions. In remote or chaotic environments, those steps are often impossible. Dried plasma bypasses many of those constraints.
European militaries have used freeze-dried plasma for decades. Research summarized in the Transfusion review shows that these products retain most coagulation activity, reduce inflammatory response, and perform similarly to fresh plasma in animal models of hemorrhagic shock. Human studies from Europe suggest faster correction of coagulopathy and fewer transfusions overall.
For Dr. Martin Schreiber, the interest is not theoretical.
As a military surgeon, he served in Iraq and Afghanistan, including leadership roles responsible for trauma systems operating under extreme conditions. Evacuation delays, supply shortages, and prolonged field care were common. Solutions had to be durable, portable, and effective long before patients reached operating rooms.
Those experiences continue to shape his civilian work. Martin Schreiber, MD, previously served as a professor of surgery at Oregon Health and Science University, where he led trauma research and education efforts. While no longer a member, Dr. Martin Schreiber remains professionally active, working in military settings, continuing research collaborations and speaking nationally and internationally.
In 2025, his invited lectures include meetings of the North Pacific Surgical Association and the Royal College of Surgeons of Thailand. He also holds an appointment as Adjunct Professor at the Uniformed Services University of the Health Sciences, where he contributes to training future military and civilian medical leaders.
At the same time, Dr. Martin A. Schreiber remains an active colonel in the U.S. Army Reserve and serves as national director of the Definitive Surgical Trauma Care Course. That role places him at the center of global efforts to prepare surgeons for life-threatening injuries in austere environments.
The civilian implications of dried blood products are growing. Nearly 20 percent of Americans live in rural areas. Many more travel through remote landscapes, national parks, deserts, and wilderness regions each year. Natural disasters and extreme weather events further strain emergency response systems.
In these settings, paramedics and flight crews often arrive with advanced skills but limited tools. Blood-based resuscitation, the standard of care inside hospitals, remains out of reach.
Dried plasma could extend that standard beyond hospital walls. It could allow emergency responders to stabilize patients earlier, buying time during long transports. Researchers are also studying dried platelet products and the possibility of dried whole blood analogs, which could further expand prehospital care.
There are still obstacles. No dried plasma product is approved for civilian use in the United States. Regulatory review, manufacturing scale, cost, and safety oversight remain challenges. But progress is underway. Canada has authorized dried plasma for military use, and U.S. companies are advancing products through development and testing. US Special Forces medics carried a dried plasma product from France in Iraq and Afghanistan.
The broader context makes the work urgent. Climate-driven disasters are increasing. Supply chains are vulnerable. Trauma does not always happen where infrastructure exists.
For Dr. Martin A. Schreiber, the question is not whether dried blood products will replace hospitals. It is whether medicine can reach patients before hospitals do.
“Distance changes everything,” he has said in professional forums. “If we can close that gap, even briefly, we change survival.”
In trauma care, survival often depends on minutes, access, and preparation. Dried blood products offer a way to bring modern resuscitation into places where it has never existed before.
For patients injured far from help, this shift could determine whether they arrive alive.
Do you want to see more of Martin? Follow him on Twitter, LinkedIn, Facebook and visit his website!